Blog - Washington, DC
Tips, Facts, And The
Latest In Dentistry

What Causes Dental Implant Failure and How Frequent Is It?
Posted in Dental Implants
Posted on November 30, 2022 by Dr. Gerald Marlin
Dental implants and their respective restorations are prone to either gum inflammation, known as peri-implant mucositis, bone loss, known as peri-implantitis, or both. As peri-implant disease progresses, it can ultimately result in the implant(s) being lost.
A systematic review and meta-analysis by Atieh et. al. included 1,497 participants and found peri-implant mucositis (gum inflammation) frequency of 63.4%, while peri-implantitis (bone loss) was prevalent in 18.8% of participants (1). On the other hand, at Elite Prosthetic Dentistry, we have a proven track record of virtually no bone loss around our implants that were surgically inserted and restored over 20 years ago. Why is that?
Why do Many Dental Implants Fail Due to Bone Loss Compared to Elite Prosthetic Dentistry?
Too many implant therapies fail because of 1) incomplete planning taking into account bone architecture and the ideal location for the implant with its restoration; 2) not using surgical guides when placing the implants resulting in poor implant placement, and 3) the fabrication of implant abutments and crowns with inadequate “emergence profile” to create a natural restoration (2,3). In our clinic, we maintain a strict quality control treatment regimen including all of these essential parameters.
Illustrating Why Inadequate Positioning of Dental Implants Causes More to Fail

In Fig. 1, we see implants #13 and #14 that are positioned inadequately close because they were not predictably inserted using a surgical guide generated from the virtual planning. As a consequence, the implant abutment in #13 was not completely inserted, leaving a gap (fig. 1 yellow arrows) that can harbor bacteria and lead to peri-implantitis. Furthermore, the dental crown on implant #14 is over-contoured, making it difficult to clean and causing it to be more plaque retentive, which can cause peri-implant mucositis (gum inflammation), while implant #15 was not restorable.
How Implant Specialists Determine the Ideal Positioning
All implant therapy starts with a CBCT scan to determine the bone width, angulation, and density. This extensive and phased analysis aids in deciding whether the implant site needs ridge augmentation (i.e. bone grafting) prior to implant placement. This is completed by performing a virtual reality simulation of “placing” the implant in the ideal position over the CBCT scan.
Subsequently, a precise surgical guide is fabricated from the virtual plan that provides the exact and ideal position during surgery (2). When planning the implant placement, we make sure that the best gingival (gum) tissue has been achieved to protect the implant. When ready for implant restoration, our In-House Lab Technician will create the ideal, natural emergence profile without any interferences from misplaced implants.
Illustrating Dental Implants with Optimal Positioning
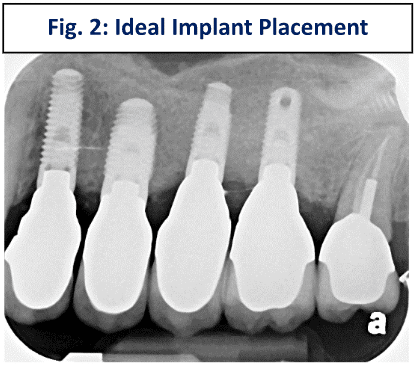
In Fig. 2, we see implants ideally situated because they were seated using a CT scan-generated surgical guide, which allowed crowns with the proper emergence profile to be easily created (Fig. 3).
As we’ve detailed here, without proper planning and precise placement of dental implants, there is a higher degree of the potential for implant failure, and corresponding negative impact on your oral health due to gum inflammation and bone loss. If you are experiencing a failed dental implant, or are considering implants, we encourage you to schedule a 1on1 consultation with one of our prosthodontists, and learn about the right treatment plan for your long-term implant success and health.
References:
- Atieh MA, Alsabeeha NH, Faggion CM Jr, Duncan WJ. The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol. 2013 Nov;84(11):1586-98. doi: 10.1902/jop.2012.120592. Epub 2012 Dec 13. PMID: 23237585.
- Abdelhay N, Prasad S, Gibson MP. Failure rates associated with guided versus non-guided dental implant placement: a systematic review and meta-analysis. BDJ Open. 2021 Aug 18;7(1):31. doi: 10.1038/s41405-021-00086-1. PMID: 34408127; PMCID: PMC8373900.
- Gomez-Meda R, Esquivel J, Blatz MB. The esthetic biological contour concept for implant restoration emergence profile design. J Esthet Restor Dent. 2021 Jan;33(1):173-184. doi: 10.1111/jerd.12714. Epub 2021 Jan 20. PMID: 33470498.

Through this commitment, Dr. Marlin provides his patients with long-lasting (35 years vs. the national average of 7-10 years) aesthetic restorations so that they have virtually no future problems.
As such, he is a leading specialist in dental implants, cosmetic dentistry, sedation dentistry , and restorative dentistry in the Bethesda–Chevy Chase, Northern Virginia, and Washington DC Metro Area. He has inserted and restored over 3,600 dental implants.





